A genetically modified fungus passed through mosquito sex could revolutionize malaria prevention by killing females before they transmit the disease.
Every evening in Burkina Faso, as the sun dips below the horizon, the air comes alive with swarms of mosquitoes — tiny, humming harbingers of one of the deadliest diseases known to humanity. Malaria still kills over 600,000 people every year, most of them children in sub-Saharan Africa. But now, a bold and almost fantastical new strategy could flip the script: a genetically modified fungus, passed through mating, that kills female mosquitoes in less than two weeks.
This isn’t the plot of a sci-fi novel. It’s a real-world breakthrough by a global team of researchers led by the University of Maryland and the Institut de Recherche en Sciences de la Santé in Bobo-Dioulasso. Their goal? To weaponize mosquitoes’ own mating behavior to decimate the very species that transmits malaria.
How this biological weapon works
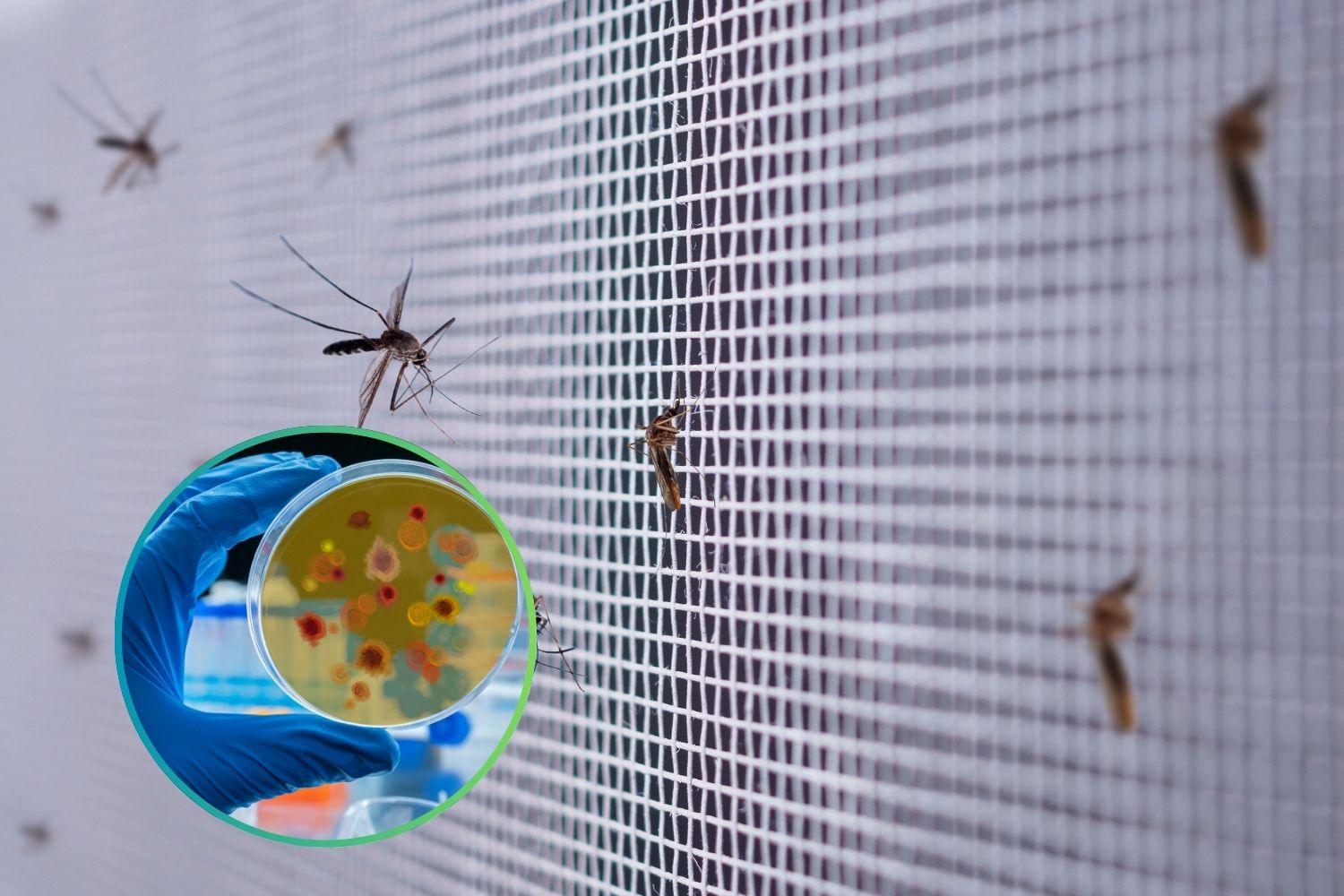
The star of the study is Metarhizium pingshaense, a fungus already known for being lethal to insects. But the researchers took things a step further: they genetically engineered it to produce a hybrid neurotoxin. It’s deadly to mosquitoes, yet harmless to humans, animals, and other species.
Here’s the twist. Male mosquitoes are dusted with spores of this modified fungus and then released into semi-natural environments. Once free, they mate as usual — and in doing so, infect the females during copulation. The results are striking: 87% of infected females died within 14 days, compared to only 4% in the control group.
Even more impressive, the fungus doesn’t change mosquito behavior. Females don’t avoid infected males. On the contrary, they mate just as frequently. This quirk makes the approach highly effective. Males remain infectious for at least 24 hours, enough time to spread the spores to multiple partners.
As Professor Raymond St. Leger, an entomologist at the University of Maryland and co-author of the study, puts it:
“While insecticides are losing effectiveness, this approach hits mosquitoes where it hurts: reproduction. That’s exactly where we strike.”
From lab to field
Published in Scientific Reports, the study was carried out in Burkina Faso, not just to test a theory but to seek real-world solutions. Researchers compared two strains of the fungus: the wild type and the genetically modified version. Only the latter reached the critical mortality threshold needed to have any real impact on malaria transmission.
One key point: the infection spreads only through mating. Simply being in the same space isn’t enough to contaminate a female mosquito. That makes the method highly targeted and selective, with minimal risk of unintended consequences.
It’s a clever workaround to a growing problem. Mosquitoes are changing their habits to dodge our defenses — for example, feeding outdoors rather than indoors where insecticide-treated nets are common. This fungus bypasses such behavioral adaptations entirely.
Even better, the fungus’ neurotoxin disrupts the mosquito’s ability to detect insecticides, making survivors more susceptible to chemical treatments. “It’s a double hit: it kills them, and if it doesn’t, it weakens them,” St. Leger explains.
The road to large-scale application
Still, we’re not there yet. Before we think of releasing clouds of infected males into the wild, there are logistical, scientific, and ethical hurdles. Larger-scale field tests are needed. Ecological assessments must be made. And yes, even seemingly minor factors — like release timing (at dusk) or the sun’s position relative to the site — can influence success.
There’s also the ethical dimension of introducing a sexually transmitted infection into natural ecosystems, even if the victims are mosquitoes. Yet, the stakes are incredibly high.
Malaria still kills
Despite decades of interventions — from pharmaceuticals to bed nets — malaria remains a leading cause of death in many African countries. By some historical estimates, mosquitoes may have been responsible for half of all human deaths ever recorded, due to the diseases they carry.
Now, even artemisinin, one of the main anti-malarial drugs, is losing ground as parasites develop resistance. Mosquitoes, too, are becoming resilient to conventional insecticides. We need new tools, tools that are smart, targeted, and adaptable.
That’s where this fungus enters the arena. It may soon be used alongside existing techniques like the Sterile Insect Technique (SIT) or Wolbachia-infected mosquitoes, which also aim to interrupt malaria transmission.
It’s a biological arms race. For every move we make, mosquitoes evolve. But for once, this fungus — transmitted during the very act that ensures their survival — could tip the balance in our favor.
In the dusty heart of Africa, among the fields and villages where malaria claims lives daily, a microscopic fungus might just be the unlikely hero we’ve been waiting for.
