Artificial intelligence: a blessing and a curse? It certainly has its limits and its “dangers” but today we know that it can help defeat antibiotic resistance, one of the main causes of death in the world, with shocking data that, going forward at this rate, will only get worse
Artificial Intelligence (AI) could play a critical role in the global battle against antibiotic resistance, one of the leading causes of death worldwide—a crisis projected to worsen drastically unless urgent action is taken.
Antibiotic resistance: a deadly comeback
Antibiotic resistance is a global health threat with the potential to throw humanity back to a time when routine infections were fatal—something we thought we had left behind nearly 80 years ago.
Bacteria that were once easily treatable are evolving to resist existing antibiotics, and new superbugs are emerging. Some strains have become virtually untreatable.
According to research published in The Lancet, more than 1.2 million people died in 2019 as a direct result of antibiotic-resistant infections.
Even more alarming: 4.95 million deaths were associated with such infections, even when the resistance wasn’t the direct cause. Antibiotic resistance is already one of the world’s top killers—and we’re only at the beginning.
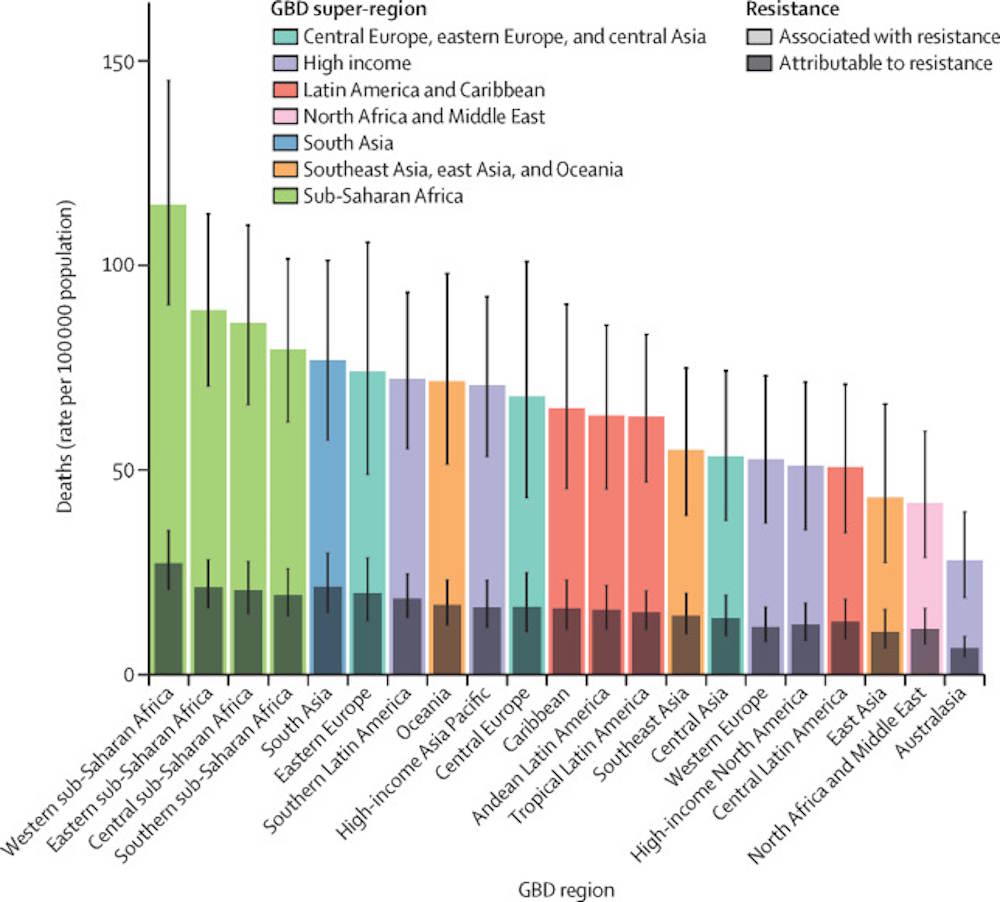
©The Lancet
What’s driving this crisis?
There are multiple causes behind the rise of antibiotic resistance. Chief among them: overuse in humans and in livestock farming.
Antibiotics have saved millions of lives since Alexander Fleming discovered penicillin in 1928. But Fleming himself warned that misuse could backfire—under-dosing or premature discontinuation of antibiotics, for example, can foster the rise of resistant bacteria.
Antibiotics should only be used when truly necessary—but that’s not what’s happening.
Today, antibiotic use remains sky-high, especially in agriculture. In industrial farms, animals are often given antibiotics preemptively, even when they’re not sick—and, disturbingly, many of these drugs are the same ones used in human medicine.
These farms are also hotbeds for infection due to overcrowding and poor living conditions. This creates a perfect storm for resistance to thrive.
Let’s not forget: we consume these animals and their products—meat, milk, eggs—while their waste reintroduces antibiotics into soil and water systems, further contaminating our ecosystem.
A 2014–2018 study by the European Centre for Disease Prevention and Control (ECDC) confirmed that while antibiotic use in livestock has declined, human consumption has not.

©ECDC/EFSA/EMA (2021)
And a follow-up ECDC report showed that antibiotic usage spiked again after the COVID-19 pandemic—proof that we’re failing to learn from past mistakes.
Can AI help turn the tide?
Despite its controversies, AI holds immense potential across scientific disciplines, including in the fight against antibiotic resistance.
“AI can be used to predict antibiotic resistance epidemics,”
a review led by Jiangxi Cancer Hospital & Institute (China) reveals.
Discovering new antibiotics is a slow, expensive process—developing just one can cost up to $1 billion and take as long as 10 years.
And here’s the paradox: pharma companies want returns on investment, but the medical community urges minimal use of new antibiotics to prevent resistance. There’s no profit in moderation.
That’s where AI can make a difference.
AI systems can analyze clinical data, genomic sequences, microbiome information, and epidemiological trends to:
-
Identify new antibiotic compounds
-
Repurpose existing drugs
-
Explore combination therapies
-
Drastically cut the time and cost of preclinical research
AI-assisted clinical decision-support tools can also help health professionals prescribe more responsibly, countering the rampant overuse we still see today.
“[Some AI models] are accelerating the discovery of new antibiotics,”
confirms a January review,
“helping to strengthen the preclinical pipeline […] With broader AI integration, its role in refining infection treatments and improving antibiotic stewardship is set to become essential in fighting antimicrobial resistance.”
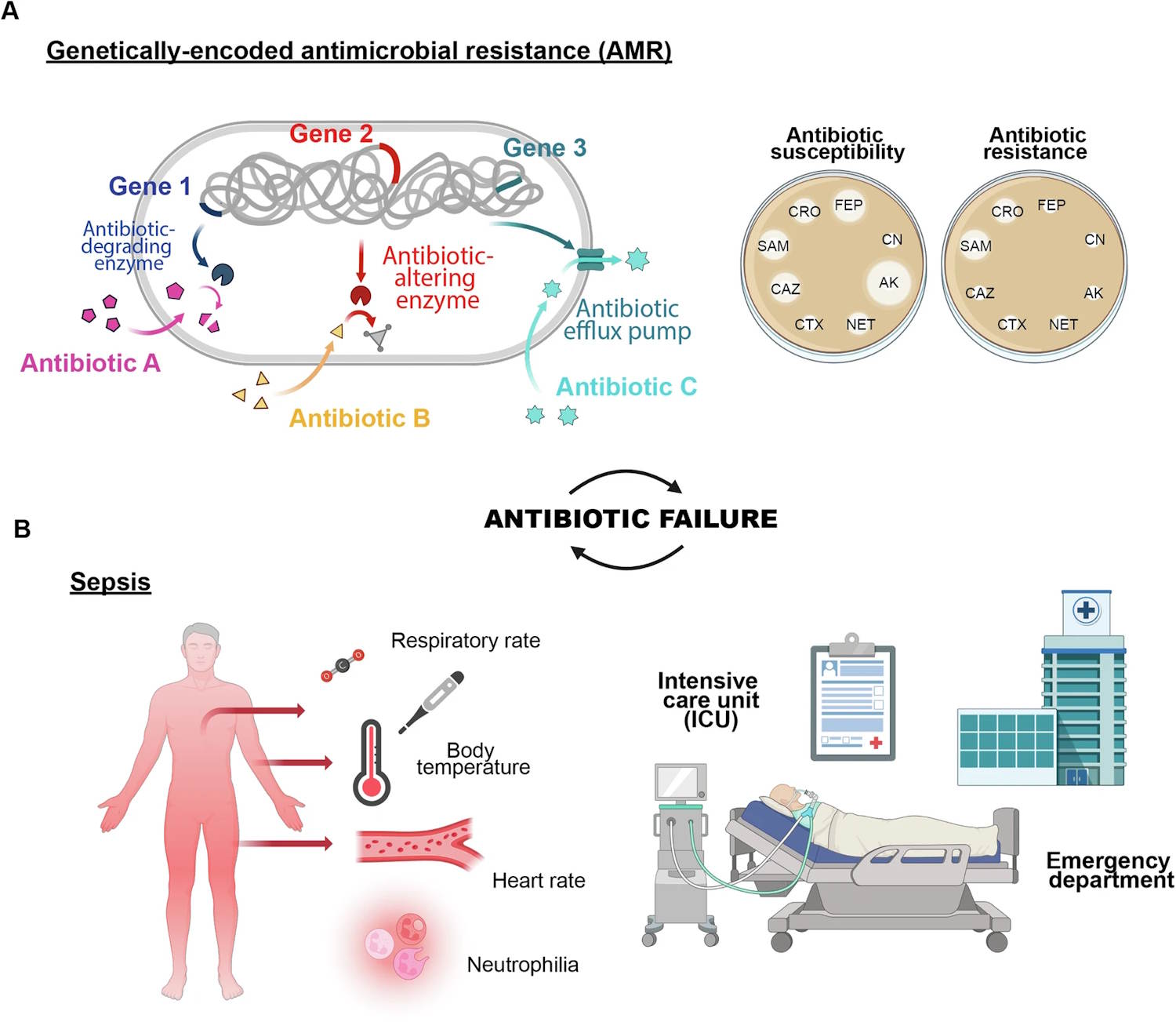
©Nature
Not a silver bullet—yet
Even so, scientists acknowledge AI is no magic fix. Several hurdles remain:
-
Data accessibility is limited, affecting AI’s effectiveness across populations
-
Ethical issues such as informed consent, privacy, and algorithmic bias need urgent attention
-
Most AI models today are trained on unbalanced datasets, raising questions about reliability
“AI models must be developed using diverse, representative datasets to avoid perpetuating bias and ensure fair, accurate results for all patients,”
researchers emphasize.
Despite its limits, AI is the direction the scientific community believes we must take. The stakes are too high to delay.
Sources: Computational and Structural Biotechnology Journal / Nature
